You walk into the ER expecting answers and leave feeling more alone than when you arrived. When a staffer asks, “What did you expect us to do?” you realize the system treats urgent moments like a triage line, not a full solution. You need clear options, realistic outcomes, and practical next steps — not platitudes.
This piece shows what actually happens when the emergency room can’t fix the underlying problem and how that gap forces you to make hard choices afterward. You’ll see where the system falls short, what to ask for in the moment, and how to start rebuilding stability once you step out of the hospital doors.

When the Emergency Room Isn’t Enough: What Really Happens
You may find the ER fast, chaotic, and focused on immediate physical danger rather than long-term mental-health support. Expect short assessments, limited beds for psychiatric care, and transfers or referrals that can feel like being bounced around.
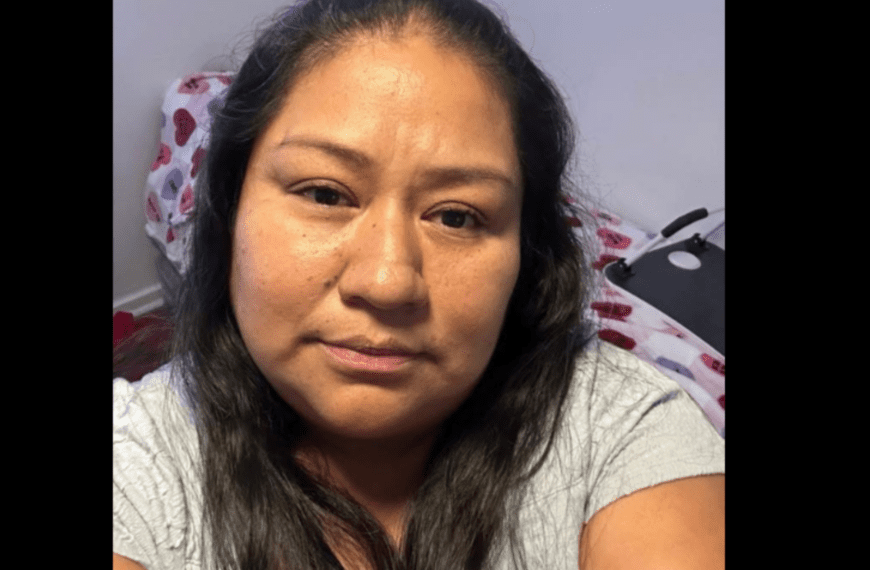
A Mother’s Experience Reaching Breaking Point
You drove to the ER because your child had stopped eating, was withdrawing, and threatened self-harm after weeks of worsening depression. Staff triaged the physical vitals quickly, then placed you in a curt intake room for a mental-health screening that lasted 10–15 minutes.
You described history, medications, and safety concerns. A nurse asked whether your child was an immediate danger; you said yes, and were told to wait for psychiatric evaluation.
The wait stretched hours. You watched other medical emergencies take precedence. When a psychiatrist finally saw you, the options presented were limited: inpatient psychiatric admission, outpatient follow-up, or referral to an emergency mobile crisis team — with beds unavailable nearby.
How Emergency Room Staff Respond to Mental Health Crises
ER staff prioritize life-threatening physical issues first, then use brief mental-health screens like the Columbia-Suicide Severity Rating Scale (C-SSRS) or quick risk questionnaires.
Psychiatric clinicians in the ER perform focused risk assessments, check for intoxication or medical causes, and decide on admission vs. safe discharge with follow-up. Resource limits shape those decisions: bed shortages, insurance constraints, and local psychiatric capacity matter.
De-escalation, short-term medication for agitation, and safety planning are common immediate steps. If no inpatient bed exists, staff often rely on crisis teams, outpatient appointments, or social services to arrange next steps.
Communicating Needs and Expectations in the ER
State your specific safety concerns and recent behavior clearly: dates, times, any threats, and whether access to means exists. Use concrete phrases: “My child said yesterday they would hurt themselves,” or “They stopped taking medication two weeks ago.”
Ask direct questions: “What criteria will you use to decide admission?” and “How long should we expect to wait for a psychiatric evaluation?” Request names and roles of staff involved, and get a timeline for next steps.
Bring documentation: medication lists, recent notes from therapists, school behavior reports, and previous hospitalization records. If you feel dismissed, remain calm but persistent: repeat key facts, ask to speak to the supervising physician, and request social work or case-management involvement.
What to Do When You Feel Dismissed
If staff minimize concerns, document the interaction: time, staff names, and what was said. You can request a second psychiatric opinion or ask to speak to the charge nurse or attending physician.
Use your phone to record factual details if allowed by local law, or keep written notes immediately after conversations. Ask for written discharge instructions and the contact information for crisis follow-up or community mental-health clinics.
If discharge occurs without an adequate plan, call local crisis hotlines, mobile crisis units, or child/adolescent psychiatric triage lines. Consider contacting your child’s outpatient provider to expedite emergency follow-up and, if necessary, file a formal complaint with the hospital to prompt review of the case.
Coping After the Emergency Room Visit
You’ll need practical next steps and emotional support to handle follow-up care, paperwork, and the stress that stays with you. The paragraphs below focus on who to contact, what to plan, and how to learn from the visit so you can feel more prepared.
Finding Support Beyond Hospital Walls
Start by listing people and services you can call within 24–48 hours: your primary care provider, the child’s pediatrician, a crisis line, and a trusted friend or family member who can help with childcare or errands. If the ER discharged medications or follow-up instructions, call the prescribing clinician or pharmacy to confirm dosages and side effects so you aren’t guessing.
Use community resources: local health departments, school nurses, and parenting support groups often offer low-cost counseling or case management. If finances or insurance are barriers, apply for social work support from the hospital or contact your insurer’s nurse line to learn covered options.
Make one or two concrete commitments this week — schedule the follow-up appointment, arrange transportation, or set up temporary help for household tasks. Small, specific actions reduce the feeling that everything is urgent at once.
Building a Personal Action Plan
Write a short, prioritized checklist for the next seven days: medications and dosing times, follow-up appointments with dates and phone numbers, symptoms that require immediate return to care, and who has keys or can pick up prescriptions. Keep this list on your phone and a printed copy where caregivers can see it.
Create an emergency-contact card for the patient with allergies, current medications, and primary clinician information. Share it with sitters, school staff, and whoever might take the child to appointments. This prevents repeated explanations and speeds care if something changes.
Set aside 30 minutes each evening to update the checklist and note any new symptoms or questions for clinicians. That habit reduces missed details during busy days and prepares you for follow-up calls or visits.
Learning from the Experience and Moving Forward
Identify one system failure you encountered (communication, wait times, unclear instructions) and one personal change you can make next time (bringing a written list, asking for a printout, designating a family spokesperson). Small adjustments improve control and reduce repeated stress.
Document the visit: date, names of clinicians you interacted with, treatments given, and any diagnostic results. This record helps when calling for clarifications, appealing insurance decisions, or briefing new providers.
Consider a short-term coping strategy for yourself: two deep-breathing exercises to use during stressful moments, one evening off where someone else handles chores, or a brief check-in with a therapist or peer support line. You don’t need to fix everything at once; pick one manageable step to protect your own wellbeing.
More from Decluttering Mom: